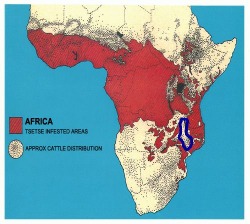
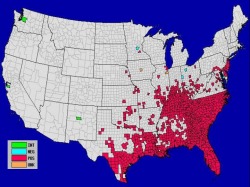
On opposite sides of the world in 2009, two vector-borne diseases that we thought were under control - dengue fever in the Florida Keys and Human African Trypanosomiasis (AHT, more commonly known as African Sleeping Sickness) in northern Malawi - returned. AHT is one of the most dreaded tropical diseases, with good reason - it is invariably fatal in the absence of proper treatment. Over 60 million people in sub-Saharan Africa are at risk and 50,000 die each year. The main vector of AHT is the tsetse fly, and control efforts have focused on eliminating this insect from endemic regions. During the 1980's and 1990's, a successful vector control program virtually eliminated the tsetse fly from Malawi, but as the disease burden decreased, funding stopped and now it appears that they fly has returned to northern Malawi. The return of the tsetse fly isn't just bad for humans - the fly can also carry a trypanosome that fatally infects cattle, which has a severe impact on the local economy. The economic impacts can be just as devastating - a Malawian villager reported, " Our colleague last year lost almost all his cattle totaling 30 head and remained with only two. We are worried because everybody is losing livestock. The flies are bringing poverty here." Dengue fever - also known as "breakbone fever" for the severe pain caused by the first infection - is the most common vector-borne viral disease worldwide. The first infection is rarely fatal, but there are four different dengue serotypes. Infection with one serotype confers immunity to that serotype, but if someone who has already been infected with one dengue serotype is infected by a different serotype, dengue hemorrhagic fever, a life-threatening illness, can result. In May 2010, the Centers for Disease Control and Prevention (CDC) announced the first locally acquired case of dengue Fever in the United States since 1946 - and that there had likely been an ongoing outbreak of dengue in the Florida Keys since 2009. A serosurvey found that up to 5% of all Florida Keys residents have been exposed to dengue. Yes, you read the first part of that sentence correctly - we eliminated dengue from the United States when we eliminated malaria (both using vector control strategies) in the mid-40's, and now it's back. The Florida Keys are a major tourist destination, and the main fear is that dengue will spread from the Keys to the rest of the United States when travelers return home. Many of the mosquitoes in the United States are capable of transmitting the virus, so the possibility of spread is a real concern. The map below shows the distribution of Aedes albopictus, one of the main vectors of dengue, in the United States. It is present in all of the counties in red, and absent from those in blue. Gray counties represent those that the Division of Vector-Borne Infectious Diseases (DVBID) didn't have the necessary funding or manpower to survey. These two outbreaks follow the same pattern - successful vector control programs resulted in the elimination of a deadly disease, and the success of these programs led many to conclude that they were no longer necessary. The problems posed by these two outbreaks are similar, but the official responses couldn't be more different. In Malawi, the return of the tsetse fly was front page news for the Sunday edition of the national paper, while news of the dengue outbreak in the United States was somewhat more difficult to find (the New York Times ran a nice article on the subject). The Malawian government and local officials have discussed the outbreak openly, asked for help, and are proposing to fund a control initiative. In contrast, the United States has imposed severe budget cuts on the CDC, forcing the closure of the DVBID (the same division that warned us of the problem), and health officials in the Keys are denying that dengue is a problem. Which country's policies seem more sensible? More on the dengue outbreak can be found at: White Coat Underground TIME
 I'll be spending my summer internship in Blantyre, Malawi, where I'll be working on a few projects. My office is in the Malaria Alert Centre, which is conveniently located next to the central hospital (where one of my advisers works) and also houses the Blantyre Malaria Project, with whom I'm collaborating on a project that is trying to develop a diagnostic algorithm to differentiate pediatric patients with bacterial meningitis from those with cerebral malaria. Both diseases have very similar symptoms and a high mortality rate, but unfortunately they both require different treatments. Complicating the situation, many health care centers (and even some district hospitals) in Malawi don't have the resources that they need to perform even basic lab work (in some cases they are unable to determine hematocrit or blood glucose), so this algorithm would ideally be based on 4-5 clinical observations that don't require sophisticated equipment. While I'm in Malawi I'll also be collaborating on a project to determine the burden of cancer in Malawi - we take it for granted in the US that we know how many cancer cases occur each year, and what the most common types of cancer are, but that information has not been systematically collected for Malawi, which makes it difficult to allocate health care resources to where they are needed. I share my office with two other researchers - an MD/PhD studying cerebral malaria, and a post-doc working on a device to measure the size of a hole that red blood cells infected with malaria can pass through. We have a fourth seat in our office which visiting researchers and professors will often use when they need a place to sit and work. It's a humble office on the second floor that is well-supplied with tea, coke, and various snacks (including the tasty but unfortunately named "Salticrax" cracker). The office looks out over fields and the noise from people working will drift in (it's the cooler dry season and our windows stay open during the day), the MAC insectory, where they raise mosquitoes (and the reason we have to close our windows when it gets dark), and across to the Malawi Liverpool Wellcome Trust. Combined, it's a nice view of both average life in Malawi and sophisticated research institutions, highlighting the need for research on infectious disease and the hope that research here will one day lead to better care.
After nearly 40 hours of continuous travel through three countries, including 3 flights, 2 (long) layovers, and a volcano scare, I've finally made it to Blantyre, Malawi, where I'll be working on my summer internship. Jet-lagged and confused, I landed in Lilongwe, the capital of Malawi, where I met a staff member from the Malaria Alert Center who happened to be in Lilongwe for sample collection and drove me down to Blantyre.
The road from Lilongwe to Blantyre was technically a highway, but not what you or I think of as a highway. Highways in Malawi are used by everyone - pedestrians and bicyclists often outnumbered the cars, and as it got darker I began to realize why traffic accidents are a leading cause in sub-Saharan Africa (hint: horns are not always effective at getting a cyclist or pedestrian to scoot over quickly). Most stalls, selling everything from fruit to cell phones to birds on a stick (fun fact: you can buy 5 roasted birds for 100 Kwacha, less than a dollar) set up right along the roadside - there are no real exits or even places to pull over safely off the road.  The scenery was amazing. What struck me first is how different everything is - the crows here have a whit torso, but otherwise look like the crows at home and the trees look different, although I can't quite put my finger on why that is. The daily life in Malawi is, obviously, very much not like that in America, and it's easiest to see in how young the population is (most people look to be younger than 25) and by how much work the children have to do. I saw at least 20 kids under the age of 8 herding goats and cattle on the side of the road - one 6-year old was able to herd 20 cattle with just a stick and lots of running. So after the trip, I'm finally settled in to the guesthouse in Blantyre and ready to start my summer internship - I can't wait.
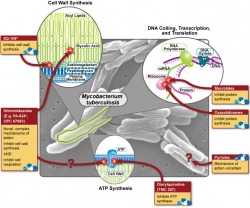
The Office of Public Health Practice hosted their annual symposium on Wednesday, and the theme was "Can the World be TB Free"? I only had a chance to attend one of the talks (by Dr. Joseph McCormick), which dealt with the rising problem of multi-drug resistant tuberculosis ( MDR-TB) and how our treatment strategies of TB may have helped this new disease to emerge. In what is sadly a familiar story for many bacterial diseases, the discovery of streptomycin (the first antibiotic that was effective against TB) was hailed as the first step in the elimination of the disease, but as time as passed the drug has become less and less effective, forcing us to search for new treatments. In the wake of the HIV/AIDS epidemic, TB has exploded and the growing problem of antibiotic resistance makes treating these people very difficult. So why does drug resistance happen, and how is it our fault? There are about 10 million (or 10^7 if you're feeling scientific) individual tuberculosis bacteria living in each cavity. About one bacteria out of every 10-100 million will randomly develop a mutation that confers resistance to any one of the two major first line drugs, rifampin and isonazid. These mutations are quite rare, but given that bacteria are nothing if not effective reproducers, it is safe to assume that approximately one bacterium per cavity is resistant to rifampin, and that another is resistant to isonazid. This situation may not sound all that bad, but consider what would happen if the patient were to be treated with rifampin alone - every single bacterium would die except for the one that had developed resistance. This bacterium is now presented with perfect growth conditions - no competition and lots of food - so it begins to multiply, and after a few days have passed, 10 million bacteria live in the cavity again - but this time all of them are resistant to rifampin. Given the large number of bacteria involved, it's now reasonable to expect that one of these resistant bacteria will then develop a resistance to isonazid, and following another single-drug treatment cycle, MDR-TB is born.
While browsing the interweb, I came across this video by Hans Rosling - probably the most amusing statistician alive today (and no, that's not an oxymoron).
Dr. Rosling teaches International Health at the Karolinksa Institutet (like Harvard, but in Sweden), and is also the Director of the Gapminder Foundation. Gapminder has some more amusing videos on their site and they take health issues, like HIV/AIDS, and present them in an entirely new context. What I especially like about the site is that they recognize that the issues are complex and that simple solutions probably don't exist (you can see this at the end of the above video when he says that he supports the media coverage, but warns us not to read into it too much).
So what exactly is public health? If you've ever wondered about this question, you're not alone - the Association of Schools of Public Health realized about a year ago that most people don't really have any idea what public health professionals do, so they made this handy website and the video below. ( Link to the video in its original context.) One of the coolest parts of this campaign: you can get the stickers for free! I like the idea of the ASPH's campaign and think it's great that the video shows a lot of public health's "hidden" aspects, but I wish that the video would show some of the dramatic effects that public health has had on society. While public health is a very broad field, it doesn't include everything (although it's a fun game to try to find some connection to public health in everyday objects - think "Six Degrees of Separation" for public health dorks). The best example is smoking - once it became clear that tobacco smoking was a major health hazard (from epidemiologic research), programs to help people quit started (thanks to Health Behavior and Health Education), and eventually policy changes were made (courtesy of Health Management and Policy) so that smoking is now banned in public places in most states (MI recently passed such a law). Other examples of changes made by public health professionals are as basic as the regulation of drinking water and ensuring that our food supplies, especially meat, remain disease-free. Going back to infectious diseases, the national vaccination program has eliminated almost all of what were formally the "childhood diseases" - no-one born in my generation has had to experience widespread polio, measles, or whooping cough outbreaks. (A list of the 10 greatest public health achievements is found here). So as a tool for raising awareness, the video is great, but I hope that it encourages people to look deeper into public health. There really is something for everyone in this field, from microbiology nerds (like me) to policy wonks (how else would we get public health laws passed?).
I have a confession: for a long time, I was pretty unclear on what public health, much less epidemiology, actually was. Given the state of public health in the media (you only hear about it when something goes horribly wrong...), it's not all that surprising. However, we have public health to thank for many of the things that we currently take for granted - like the idea that smoking is dangerous and the elimination of many once-dreaded childhood diseases like measles and polio. My interest in the field of public health in general, and epidemiology in particular, began when I read Richard Preston's The Hot Zone and I continued to be inspired by popular accounts of how epidemiology interacts with modern life in very hidden ways.  If you think that you might have even a passing interest in public health, I encourage you to check out the two books above. They each highlight why epidemiology is such a fascinating field, but they approach it from two different directions. My favorite of the two is The Hot Zone, which follows the US Army's attempt to contain an Ebolavirus outbreak (yes, that Ebola) in Reston, VA (yes, the one next to Washington D.C.). The book has some fairly surreal scenes - like an army clean-up unit staring at a busy playground while the suit up to enter an infected monkey house in secrecy - and it may or may not have contributed to a slightly romanticized view of what epidemiologists actually do (sadly, so far we've not been mobilized to contain any outbreaks and I've not had to run tests on infected monkeys). But the book does highlight the extraordinary level of surveillance that our public health officials must maintain and the variety of situations that they need to be prepared to handle.
 Stephen Johnson's The Ghost Map takes a different approach to public health - how it can be used to clean up after a disaster. In the mid-19th Century, people began flocking from the countryside to the city, creating the lifestyle that most of us now take for granted. The population of most major urban centers exploded, and to borrow a phrase from Johnson, London was "... a Victorian city with an Elizabethan infrastructure." The recent conquest of India brought a different kind of immigrant to England's capital - Vibrio cholerae, a nasty bacterial species that causes cholera, which produced extremely severe diarrhea. From 1853-54, a cholera outbreak killed 10,000 people in London, and The Ghost Map tracks how the cause of this disease was discovered and how the later public health improvements helped create what we think of as modern urban infrastructure.
Both books are great reads, especially if you think you might be interested in this thing called "public health" - and yet they only scratch the surface of one aspect of one part of one discipline of the whole. There's lots more good books out there - The Coming Plague comes to mind, and I'm sure that some of you may have suggestions of your own.
In 1700, the Italian physician Bernadino Ramazinni published the first book about occupational epidemiology. His method was simple: based on trends observed in his clinical practice, he studied his patients' worksites and found that certain diseases were correlated with specific exposures, including heavy metals and dust with cancer in miners and industrial workers, and bad posture with pain in weavers. He even looked into how the dangers of an "overtaxed mind" could cause disease in learned men.
However, his most enduring legacy is the observation that nuns had more breast cancer and less cervical cancer when compared to the general population of females living in Padua (his hometown). It was a puzzling observation, and one that he did not expect (at the time, one theory about breast cancer was that it resulted from "vigorous sexual concourse"). His explanation followed a similar line of reasoning - the breast is a sexual organ, and without regular sexual activity it would decay. Cancer was the result. Interestingly, he did not apply this same logic to the low incidence of cervical cancer in nuns, but he did propose that it was somehow related to the celibate lifestyle. As it turns out, Ramazzini was right - even if for the wrong reasons. Breast cancer is related to celibacy, but not in the way that you might think. When women become pregnant, their bodies undergo dramatic changes in hormone output, and levels of estrogen decrease markedly. Estrogen has been implicated in the development of breast cancer, and it's thought that the decline in levels brought on by pregnancy has a protective effect. Indeed, women who first become pregnant before the age of 30 have a lower risk of breast cancer than women who first become pregnant after the age of 35.
With cervical cancer, the link is even more dramatic - almost all cases of cervical cancer (>99%) are caused by human papillomavirus (HPV), a sexually transmitted disease. Since the nuns were celibate, they never acquired the virus and therefore never developed cervical cancer. Taken together, these two observations were the first inkling that modern science into lifestyle factors as a possible cause of cancer. We still use this thinking today - smoking is a lifestyle factor, and its role in the development of lung cancer is widely accepted as fact. So although Ramazzini was right for the wrong reasons, his investigation of breast cancer in nuns is one of the great early epidemiologic studies and demonstrates how epidemiology can help us to understand ways to prevent disease and puzzle out risk factors even without a firm grasp of the biologic cause.
It's hard to believe that I've completed 25% of my MPH here at the University of Michigan - time has flown by since I started the program. As short as the semester was, our winter break was much shorter (they give us all of two and a half weeks off) and now it's back to work. Seeing as it's the start of a new year and all, now is a good a time as any to look back on last semester, see what I've learned so far, and look ahead to where I hope to be at the end of this semester. To be honest, I wasn't quite sure what to expect when I started last semester (it's not as much like The Hot Zone as I'd hoped...). All in all, it was much more math-based than I thought - I was expecting more of a focus on science and biology. I'll be continuing that trend this term, as most of my courses are either statistics, study design (scientific thinking combined with applied statistics), or using math to model infectious diseases (which is much more fun than it sounds, I promise). So what did I accomplish last semester? There's a picture of the workload below (it's about a foot high). While it looks like a lot, I enjoyed (almost) every minute of it. The assignments were practical and interesting, and the vast majority of the readings were enjoyable. I'm very pleased with the program so far and looking forward to another semester.
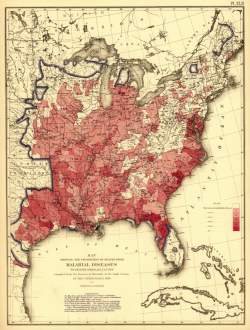
When you think about malaria, chances are high that the United States is not the first country that comes to mind. However, malaria was endemic in the US until the late 1940's, and the high prevalence of malaria in the Southeastern US is one of the main reasons why the CDC headquarters is located in Atlanta.
Malaria has a long history in the US. Until 1880 it was thought that malaria was caused by bad air ("malaria" comes from the Medieval Italian for "bad air") and it wasn't until 1898 that Sir Ronald Ross of Britain proved that malaria is transmitted by mosquitos. Our capital was built on a swamp (truly a wonder of modern urban planning) and in the summer was notorious for diseases including malaria and yellow fever.
It's easy to forget that until as recently as a century ago, much of the US was still a developing country - industrial manufacturing was low and most people lived in small towns and worked on family farms. The population density was low in many regions and low-lying fields were good farmland and ideal breeding grounds for the mosquitoes that carried malaria when they flooded. Malaria was such a problem in the US that the US Census of 1870 released a map showing areas in the US where malaria prevalence was high (see below). The map is courtesy of the US Library of Congress and can be found in its original context here. Michigan's reputation as a hotbed of malaria was well known, as the following quote from the Bulletin of the Medical and Surgical Sanitorium (Battle Creek, Michigan, 1892) shows: "But what about Michigan malaria? Unfortunately for the reputation of Michigan as a healthful State, the idea got abroad many years ago that the principal feature of its climate was malaria. Going to Michigan was considered almost synonymous with going to have a fit of the ague. It was not supposed to be possible for a person to visit Michigan or even to pass through the State without having the chills." Apart from being a mere historical curiosity, the high prevalence of malaria in Michigan served as a barrier to development - the rural regions of Central Michigan stand in sharp contrast to the well-developed Southeast and are a legacy of peoples' hesitancy to venture further inland. So how did we eradicate malaria in the United States? Public health. Even before it was known that malaria was transmitted by mosquitoes, people would clear swamps to reduce the incidence - a classic example of how you can solve a health problem without knowing the exact cause of disease if you understand the risk factors. Once we figured out that mosquitoes were the culprit, much of the eradication effort focused on their elimination. Common practices included land improvement, removal of mosquito breeding sites, and heavy insecticide use. DDT was the most commonly used insecticide, and its use in the 1940's to eliminate malaria lead to severe environmental consequences (for more, see Silent Spring). A very nice (and brief) history can be found here.
|




 RSS Feed
RSS Feed